As a new physiotherapist, Fiona Murphy found that patients sometimes responded to her gentle hands in surprising ways. They would shriek and shrink away. But, she discovered, the right words were invaluable in persuading patients to work with her and begin their recovery.

It is early 2008, and on the other side of the hospital curtain there are three beds. Each patient is awake and probably listening.
“Hi, I’m a physiotherapy student.” I point to the university crest stitched into my polo top.
I am to assess this patient and at the same time be assessed for how well I collect information about his body. I’ve rehearsed the task several times this morning: on the train; in a narrow toilet stall; and, discreetly, next to the lunchroom microwave while waiting for it to ding. It feels different now that I have someone looking at me.
Despite the patient being tucked in, we are at eye level. He’s bolstered by a pillow fort, one under each arm and another two under his head. I’ve learned that the sickest people can’t lie flat: the weight of gravity sits on their chest and the effort to draw breath is too immense.
I approach him with caution, not wanting to trespass. His hospital gown is stretched out like a tarpaulin, allowing several tubes carrying blood, bile and piss to snake out the sides. Oxygen prongs sit in his nostrils and jiggle as he greets me.
“More like physio-terrorist!” His laugh causes the containers of liquid to bubble. “Have you ever heard that one before?” His lips thin and twist into a smirk.
“No.” I hug my clipboard to my chest. It has a list of the essential things to do in a patient treatment session: wash hands before entering the room; introduce yourself; ask for consent; check blood pressure; disinfect the head of the stethoscope with an alcohol swab; listen to chest sounds; test the strength of their cough; check the consistency and colour of their mucus, and so on.
“You lot cause nothing but pain. Physio-terrorist!”
My supervisor is in the hallway, so I laugh – I don’t want to lose marks for lack of patient rapport.

“Even in warm months I have chilblains. At work, I shove my hands deep into my pockets... as well as clap and clench them. And still my patients scream as if shocked.”
On the hospital ward
After graduating from university, my first job was on an orthopaedics ward. Most patients proudly pointed to their new hip or knee buried beneath freshly stitched skin. They were chuffed, ready to roll out of bed, believing that their pain was now a thing of the past.
Once they started to move, however, the pain was always sudden, sharp and steely. This pain, I soon learn, can’t be completely dulled by analgesia – too many medications can cause complications, including excessive drowsiness. And here, the post-operation orders were strict. Every patient had to be up and moving.
The patient in front of me had knee-replacement surgery yesterday and is resisting my attempts to persuade her out of bed.
“No!” She folds her arms.
“But we need to get you up to start rehab.”
“Stop using we. It’s you. You are trying to get me out of bed. I just want to rest.”
“It’s almost lunchtime. You can’t lie in bed all day.”
My hands rest on my hips. I’m hungry, and annoyed that she has closed her eyes.
“We need to exercise your new knee.”
She flinches.
“Sorry. I mean you. You need to exercise your knee.”
“Fine!” She throws off her blanket. “You’re a cruel woman.”
I step forward, hands out, ready to assist her over the edge of the bed.
“Rack off,” she says and grimaces as she rolls onto her side. “Just look at what you’re making me do.”
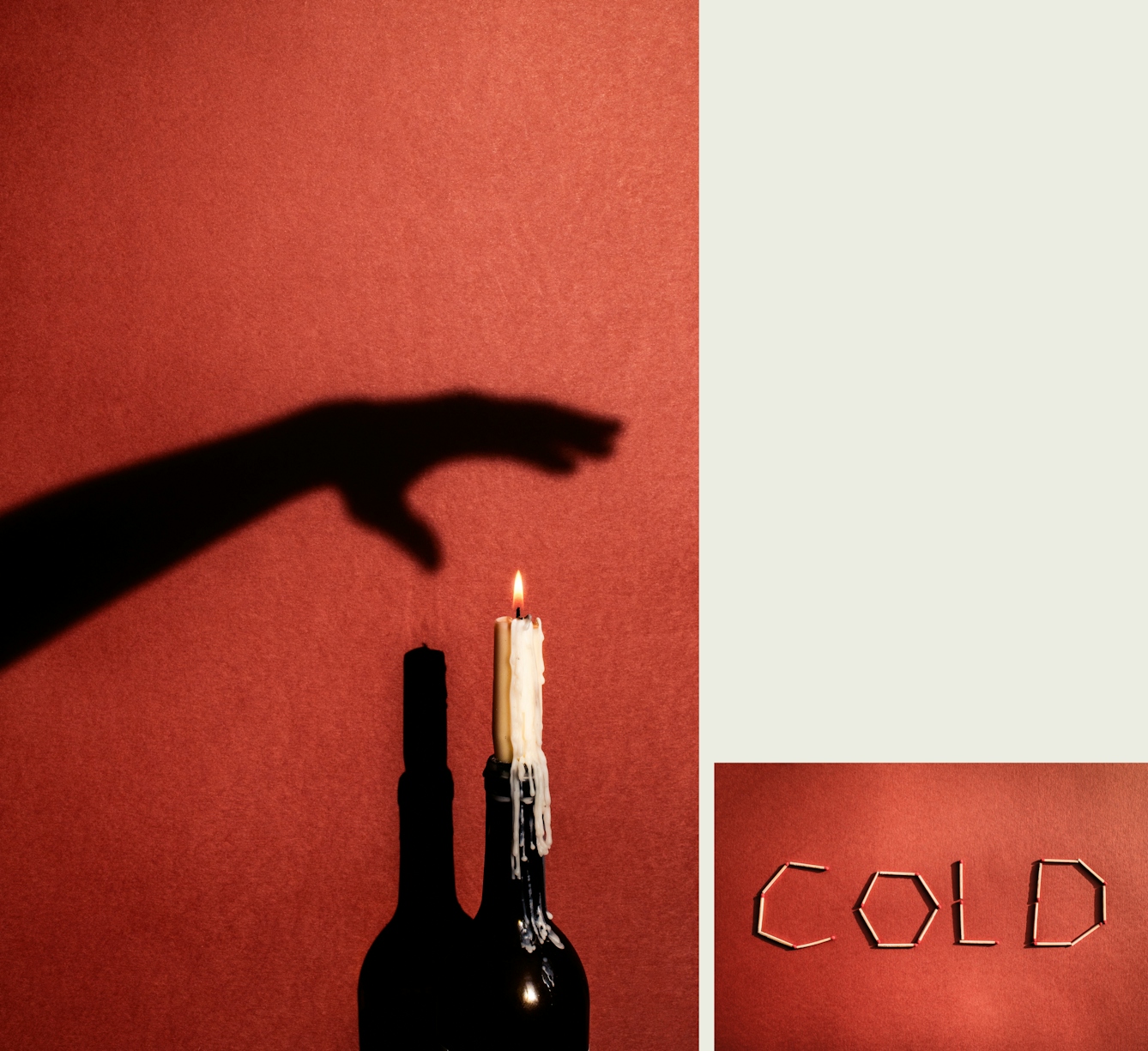
“I learned that I needed to add a warning to my script. ‘Sorry for my cold hands,’ I’d say before palpating their back or knee. ‘You weren’t joking,’ was the common refrain.”
While studying physiotherapy we had small scripts to practice. This was to ensure that we clearly introduced ourselves, confirmed the patient’s identity, explained the treatment plan, had the patient’s consent, and that we always offered empathy.
When practising with my classmates, these words felt flat and hollow as we recited them to each other. But, over time, as we began to see patients during clinical placements, they become more meaningful. We would lose marks if we missed a step in the script.
It was only when I graduated and started working that I discovered gaps in these scripts. They didn’t account for how unpredictable pain can be.
Pain is personal
“I bet you’ve never been in pain.” She stops moving and clutches her knee.
I don’t tell her about my broken bones. The reoccurring back spasms I’ve had since falling through a ceiling 17 years ago. The shrill headaches that descend weekly. Or the menstrual migraines that flatten me monthly. These are not part of the script.
“You’re doing well – you’ve just got ten more repetitions to go. You’ve got three more days until you can be discharged.”
“You have no idea how this feels.” In many ways, my patient is right. Besides studying anatomy and the biomechanics of joint replacements, I didn’t actually know what she was going through. No textbook or university tutor could fully prepare me.
If we all slipped on a banana peel and sustained exactly the same injuries, we’d ache in different ways.

“Over the intervening years, I’ve learned to be careful with the words that I use when talking to patients. You see, words can rub and burn just as much as they can soothe.”
Pain is not a linear process, with predictable start and end points. Rather, pain is personal. It’s influenced by your degree of perceived danger, and your life and medical history. And so, even if we all slipped on a banana peel and sustained exactly the same injuries, we’d all ache in different ways.
At the time, just as I was starting my career, I didn’t quite have my head wrapped around the practicalities of these concepts. But I was quickly learning that if I treated patients even with the slightest touch, many would shriek and recoil.
Handle with care
Each of my nails is ringed with red skin. Even in warm months I have chilblains. At work, I shove my hands deep into my pockets, curl them around ginger teas, knead them with cream, as well as clap and clench them. And still my patients scream as if shocked.
I soon learned that I needed to add a warning to my script. “Sorry for my cold hands,” I’d say before palpating their back or knee. “You weren’t joking,” was the common refrain.
The brain can prime the body for pain — including a cold set of hands — if given sufficient warning. Conversely, it can intensify an experience if caught off guard. And so my approach, albeit apologetic, was often enough to avoid shocking patients. But, I wondered, was there anything else I could say to help minimise my patients’ pain?
Over the intervening years, I’ve learned to be careful with the words that I use when talking to patients. You see, words can rub and burn just as much as they can soothe.
Researchers from Emory University in Atlanta have studied how the brain reacts to language. Test subjects lay in an MRI machine and listened as a researcher recited metaphorical and literal descriptions, such as — the operation went smoothly (the operation went successfully), she has nerves of steel (she is very calm), he had leathery hands (he had strong hands) — in a neutral tone with minimum inflection.
“I think about the metaphors frequently associated with injuries... I wonder how often I’ve used these common but violent descriptions without even thinking.”
The results were conclusive. Textured metaphors caused the brain to react like it was being touched.
I think about the metaphors frequently associated with injuries — wear and tear, frozen, burning, stabbing, shooting, lacerating. I wonder how often I’ve used these common but violent descriptions without even thinking. For a while I worry if all I have done is cause pain.
Stories that comfort and soothe
Now, whenever I am trying to encourage someone to move — especially when I know that it might be an uncomfortable or even painful process — I try to think of meaningful ways to explain the treatment.
Trisha Greenhalgh and Brian Hurwitz were early proponents for the importance of narratives in healthcare. In 1999 they wrote: “Narrative provides meaning, context, perspective for the patient's predicament. It defines how, why, and what way he or she is ill. It offers, in short, a possibility of understanding which cannot be arrived at by any other means.”
In the context of physiotherapy, a narrative may be as simple as saying, “Motion is lotion.” This phrase neatly reframes the idea of moving a stiff joint as a beneficial and potentially soothing sensation. It is softer and more soothing than saying, “No pain, no gain.”
Sometimes it’s helpful to remember that patient who called me a physio-terrorist, who said, “All you do is cause pain.” It reminds me that words, including my job title, can have a significant impact.
Rather than relying on scripts or clichés, I lean into open-ended questions, such as, “Can you tell me the story about your pain?” and listen hard before responding. I choose my words carefully, checking whether they place a patient at ease. Although pain is a solitary experience, treatment sessions should be a place of teamwork.
Want to find out more about our attitudes and experiences of touch? The results of Wellcome Collection and BBC Radio 4’s survey, The Touch Test, are out now.
About the contributors
Fiona Murphy
Fiona Murphy is an award-winning writer based in Australia. Her memoir about being Deaf, ‘The Shape of Sound’, is forthcoming from Text Publishing in 2021.
Camilla Greenwell
Camilla Greenwell is a photographer specialising in dance, performance and portraiture. She regularly works with Sadler’s Wells, Barbican, Candoco, Rambert, The Place, the Guardian, the British Red Cross, Art on the Underground and Wellcome Collection.

